Abstract
Conflicts of Interest in Systematic Reviews on Methylphenidate for Attention-Deficit Disorder
Alexandra Snellman,1 Stella Carlberg,1 Louise Olsson1
Objective
To compare financial conflict of interest (COI) as declared by authors of systematic reviews (SRs) of methylphenidate for attention-deficit disorder with publicly available information and in relation to risk of bias (RoB).
Design
SRs on the outcomes associated with methylphenidate for attention-deficit disorder in all ages were searched in Medline, Cochrane, Embase, and PsycInfo. The Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline was followed for the selection of relevant SRs. Two reviewers (A.S. and S.C.) independently screened open websites and recent publications for all authors of each SR, and data on financial COI were extracted. All searches followed a preplanned and similar routine. A time limit of 3 years from publication of the index SR was applied. Findings were discussed between the reviewers and repeated until consensus was reached. If no data were found for any of the authors, the SR was categorized as no COI. Two reviewers (A.S. and L.O.) independently judged RoB of the SR using the Risk of Bias in Systematic Reviews (ROBIS) tool. Any disagreement was resolved in consensus. In addition, data were retrieved on COI as declared by authors.
Results
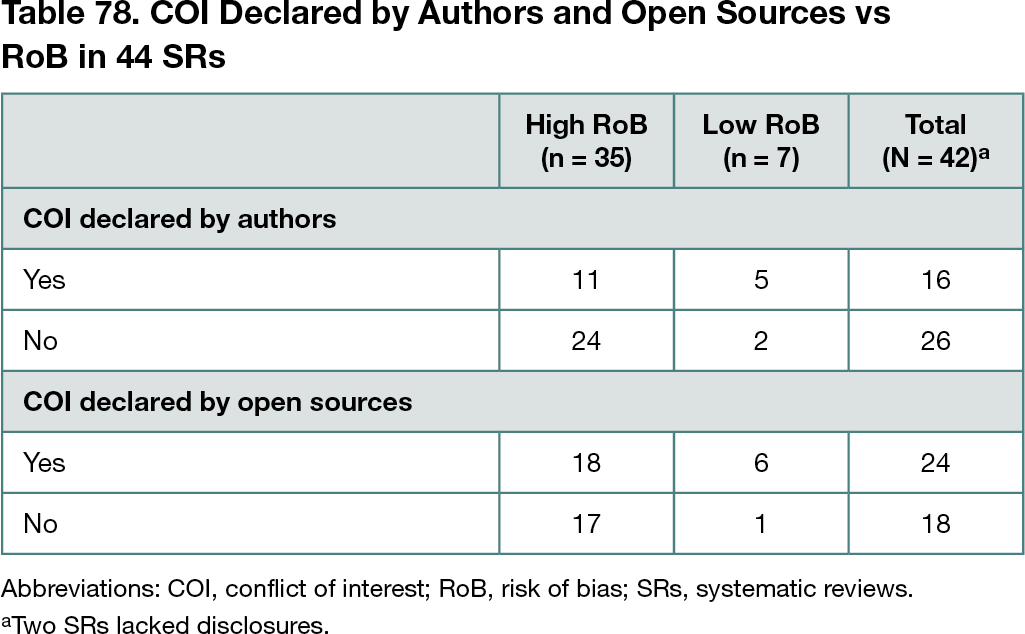
Of 651 unique publications, 44 relevant SRs published between 2008 and 2021 were included. In all, 32 SRs (73%) were based on randomized clinical trials only, 18 (41%) reported positive effects only, 15 (34%) reported both positive and adverse effects, and 11 (25%) reported adverse effects only. Eleven SRs (25%) included only studies using placebo for comparison. A meta-analysis was conducted in 26 of the SRs (59%). COI disclosure was missing for 2 of 44 SRs (5%). For 15 SRs (34%), authors declared COI, and this declaration was confirmed by open sources in all cases. For 27 SRs (61%), the authors declared no COI, but discordant information was publicly available for 8 of 27 (30%). The direction of COI for most SRs was not able to be assessed. The RoB was high in 37 of 44 SRs (84%). Of the 7 SRs with low RoB, 1 had no COI identified in open sources (Table 78).
Conclusions
The findings indicated an underreporting of COI in SRs in studies on attention-deficit disorder, and most SRs were compromised by high RoB. Owing to small numbers, no firm conclusion on the association between COI and RoB was possible.
1Centre for Assessment of Medical Technology in Örebro, Örebro University Hospital, Örebro, Sweden, alexandra.snellman@regionorebrolan.se
Conflict of Interest Disclosures
None reported.