The 10th International Congress on Peer Review and Scientific Publication
September 3-5, 2025

Our aim is to encourage research into the quality, integrity, and credibility of peer review and scientific publication, to establish the evidence base on which scientists can improve the conduct, reporting, and dissemination of scientific research.
An error occurred submitting the form. Please try again.
Submitting...
Thank you for subscribing!
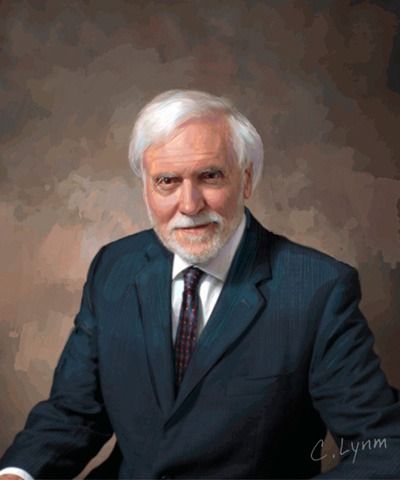
Drummond Rennie, 1936-2025 Founder of the Peer Review Congress
JAMA: Remembering Drummond Rennie—Champion of Integrity in Science and Scientific Publication
BMJ: Drummond Rennie: Tributes are paid to “prophet of peer review” after his death at 89
Retraction Watch: Drummond Rennie (1936-2025), in his own words
-
About the Congress
What? The Congress is held every 4 years and provides a forum for the presentation and discussion of research into the quality, integrity, and credibility of editorial and funding peer review, scientific and scholarly publication, research and reporting practices, identification and management of biases, transparency, reproducibility, access, publication and dissemination metrics, identification and management of threats to the integrity of science, and advances in information exchange.
Who? Participants include editors and publishers of scientific peer-reviewed journals, researchers, funders, bibliometric and informatics experts, information innovators, librarians, journalists, policymakers, ethicists, scientific information disseminators, and anyone interested in the progress of the scientific information enterprise and the quality of scientific evidence.
The Congress embraces a wide range of disciplines, including biomedicine, health and life sciences, applied sciences, basic sciences, physical and chemical sciences, mathematics, computer sciences, engineering, economics, and social sciences as well as new and emerging disciplines.